- Plastic stomachs that can vomit and mini stomachs made from stem cells
- Artificial hearts could soon spell the end of donor organ waiting lists
- Researchers have created artificial muscles that are just like the real thing
- A new bionic leg can sense when the wearer wants to walk, sit or stand
- Improved cochlear implants enable the deaf to surpass the hearing
Whether or not you are a sci-fi fan, cyborgs – a fusion of technology with human biology – capture the imagination of most people. Today’s technological developments enable us to fix, replace or enhance almost every part of the human body, including stomachs, kidneys, hearts, lungs, muscles, skin, arms and legs, and ears and eyes. These are now real science instead of science fiction, and they have many potential applications, especially for those suffering from physical disabilities. Technological and medical advances continue, and in the future, whether we like it or not, human bodies will contain at least one if not more technologically and mechanically engineered parts.
Here’s our list of ten recent cyborg-esque breakthroughs that could save – or at the very least, improve – the lives of many. Some of these can even give us superhuman capabilities.
Free trendservice
1. Plastic stomachs that can vomit and mini stomachs made from stem cells
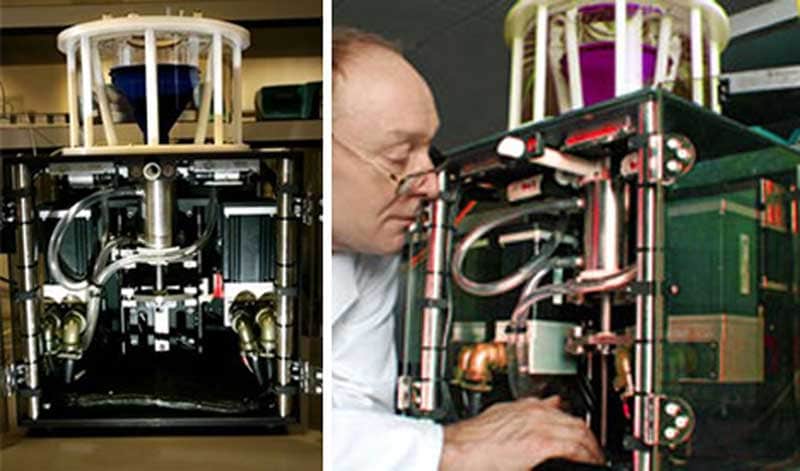
The world’s first artificial stomach was developed in 2006. Created from sophisticated metals and plastics able to withstand the corrosive enzymes and acids of the human gut, the shiny, high-tech box physically simulates human digestion. It’s being used to develop specially formulated foods to help those suffering from obesity by tricking the stomach into thinking it’s full. The artificial stomach was funded by the British government, designed by Dr. Martin Wickham of the Norwich Institute of Food Research, and cost approximately $1.8 million to create.
The plastic gut contracts and breaks up food and moves it through the process of human digestion. Its top consists of a funnel in which digestive enzymes, stomach acids and food are mixed. In a metal tube, encased in a transparent box, the food then gets ground down. The parameters of the artificial stomach are set by software, including whether it’s an adult or child’s stomach, the amount of time food stays in a specific section, as well as predicted hormone responses at the different stages. Scientists’ knowledge of what actually happens in the stomach is still very limited and the aim of the model stomach is to study the chemical and physical reactions taking place during digestion to gain insight into food structure and its effect on digestion. If we understand how food is processed in the stomach, and which part of the organ is responsible for nutrient absorption, we may be able to develop food that can manipulate the digestive process. We could, for instance, treat diabetes better if we can see how fast glucose is absorbed into the bloodstream. The artificial stomach can consume approximately 24 ounces of food with its most substantial meal having been tomato soup. “The stomach is so realistic, it is even capable of vomiting,” said Wickam.
Last year, great strides have also been made with stem cells to build so-called mini stomachs, made from minuscule clusters of human gastric tissue called gastric organoids. These developments could enable new research into diabetes, ulcers and cancer. Jim Wells, a researcher in developmental biology at the Cincinnati Children’s Hospital Medical Centre said: “Up until recently, there hasn’t really been a proper way to study diseases of the stomach. The human stomach is very different from animal stomachs. But now, with the pluripotent stem cells we can even grow transplant tissue. The challenge has been to get the cells to ‘differentiate’, in other words, turn into cells for specific organs.” With this new research, we’ve managed to identify the chemical steps that happen during cell development, when they change into specific types that form specific organs, in this case, the stomach. Still in their early stages of development, these gastric organoids could one day form replacement tissue to patch the holes formed by ulcers. The organoids could even be used to create complete stomachs. At this point, however, they are the perfect testbed for studying disease.
2. The AWAK waterless, bloodless artificial kidney ‘wearable’
The AWAK, or ‘A Wearable Artificial Kidney’, is patented sorbent technology which revolutionises dialysis. It was developed by a team of scientists from AWAK Technologies Pte Ltd., a medical technology company dedicated to transforming the lives of patients with kidney problems. The AWAK can help kidney patients undergo dialysis without having to go into the hospital. The device weighs only 1 kg, can be carried in a pouch, and works 24/7, allowing patients to live nearly normal lives and enjoy leisure activities and even sports. The AWAK is based on a treatment method called peritoneal dialysis. This is the cleaning process that uses the body’s peritoneal membrane in the abdomen. As this method of dialysis does not involve external blood circulation, it is very safe for the patient.
The artificial kidney is waterless and bloodless and functions by constantly regenerating used-up dialysate in a sorbent cartridge, so that the device does not have to depend on external fluid supply. This makes the artificial kidney a true wearable, allowing the patient freedom of movement and an enhanced quality of life.
3. “Be still, my completely artificial beating heart”
Completely artificial hearts will soon be coming to a heart transplant patient near you. Yes, biomedical engineers have recently managed to build a mechanical version of that tirelessly working muscle that beats 100,000 times a day, ensuring blood circulates through our entire body. Building artificial hearts has been attempted by various researchers since the fifties, but to date, nobody has fully succeeded. Two companies have now created permanent artificial hearts that have withstood extensive clinical trials and animal tests and are ready for human use. This breakthrough technology could mean the end of long waiting lists and people dying while waiting for a donor heart.

SynCardia
The artificial heart from SynCardia Systems, a company based in Arizona, consists of two plastic chambers, each of them bifurcated by a membrane with blood on one side and air on the other. The air is delivered to the chambers via a 6-kg air compressor with tubes through the abdomen pressing on the membranes and propelling the blood on the other side. The artificial heart already has US regulatory approval for use as a temporary solution while a patient waits for a donor heart. The company is currently enrolling patients in clinical trials to test the artificial heart as a permanent replacement option. CEO Michael Garippa says that more than 1,600 temporary placements of the artificial heart have proven that the device is safe, although the compressor is quite loud as it steadily thumps away at 120 ‘beats’ per minute. “Although it is certainly not a normal life, it is an improvement compared to what patients with heart failure have experienced up until now,” says Garippa.
Carmat
In comparison, French-based company Carmat’s system is completely silent, according to the company’s chief medical officer, Piet Jansen. Like the SynCardia, the Carmat heart also has two artificial chambers with membranes that press outward to pump blood. It uses hydraulic fluid in an implanted pump, however, instead of compressed air. The Carmat heart itself is more complex as well as larger and heavier, and the system necessitates wires emerging from the patient’s neck to connect it to a battery. However, its microprocessor can calculate the right heart rate according to the level of exertion of the patient, using built-in sensors, something the developers are very proud of. Although the first feasibility study – in which two of the four patients who tried the heart died – was not very successful, the patients in question were extremely sick to begin with. What happened during the study was therefore attributed to a failure of the body, rather than a failure of the artificial heart. A major clinical trial was recently approved by European regulators and Carmat aims to implant about twenty of its devices by the end of this year, hoping Europeans will have access to the heart as a certified permanent replacement device by next year.
4. Wearing your lungs in your backpack
Another artificial device that can transform the lives of people with severely debilitating or life-threatening conditions is the artificial lung. This device is small enough to carry in a backpack and has been proven to work in sheep. Patients with lung failure are often stuck in bed, connected to bulky machines with lots of tubes that pump their blood through an exchanger system supplying oxygen and removing carbon dioxide. Artificial lungs could be the solution for those waiting for a transplant, but they are much more complicated to make than artificial hearts. William Federspiel of the University of Pittsburgh says: “The heart is merely a pump. The lungs, on the other hand, contain an intricate and highly efficient network of air sacs through which air diffuses in and out of the blood. No technology can come close to mimicking this type of efficiency. Then there’s the challenge of pushing the blood through the gas exchanger, for which you need a pump.” Federspiel’s team has, however, managed to develop an artificial lung in which the gas exchanger and pump are combined.

5. Artificial, multifilament muscles that are just like the real thing
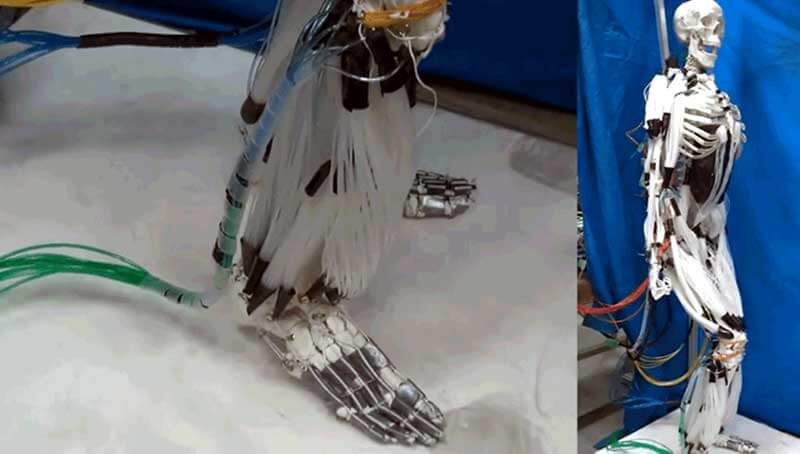
We’re not just creating artificial body parts for humans, we’re also re-imagining real body parts for use in robots. Robots are currently powered by pneumatic pistons and servos, but they make the machines extremely heavy and bulky – so much so that you will never mistake them for real human beings. If we want to create a credible humanoid, something like Terminator-style robots, however, we will have to do something about those bulky muscles. Researchers at the Robotics Laboratory of the Tokyo Institute of Technology are mimicking real human muscles by creating multifilament versions that can expand and contract when an electrical current is applied. The team managed to move the arms, legs and head of a skeleton model in a human-like way by controlling different groups of these artificial muscles. They are still quite a bit slower than real muscles, which means that self-balancing at this stage is not yet among the possibilities. The researchers are working on improving the technology, however, making hyper-realistic humanoid robots a reality sooner than you may think. And who knows, these artificial muscles may one day revolutionise our own human bodies as well.
6. Artificial skin that can detect heat like a snake
Another important part of humanoid robots that needs improving is their skin. With a thin, clear, flexible film, made from a plant-based polymer called pectin (the substance that helps jam to set), prosthetics and robots could be made to look and feel even more life-like. A group of Swiss and US researchers have now developed temperature-sensitive artificial skin that can detect body heat up to a metre away much the same way as certain types of rattlesnakes that can detect heat through pit glands containing a heat-sensitive membrane. The low-cost pectin skin, with half the thickness of a human hair, could be used in many different ways, from integration in gadgets with thermal sensors to prosthetic limbs with temperature feedback to augmenting robots with heat-sensitive skin. One of the researchers said: “the most important aspect of this project was learning fundamental mechanisms from nature. It allows us to create materials that have extreme and unprecedented properties.”

7. Bionic leg senses when the wearer wants to walk, sit or stand
In 2015, the prosthetics specialist Blatchford released the first ever integrated robotic lower limb that actually ‘behaves’ like a real human leg, signifying the start of the next generation of prosthetics. The leg was the winner of the Royal Academy of Engineering’s 2016 MacRobert Award for innovation in engineering. Since its release, the bionic leg, known as Linx, has sold hundreds of units worldwide, with Germany and the US being the main markets. The knee and foot of the Linx work together in the same way as a human leg. The limb has an array of sensors that constantly collect data on the environment in which the wearer is standing, sitting or walking. This information is collected by processors and the specially developed software then enables the limb to adapt the positions of the knee and ankle in response, meaning that the two joints are in continuous dialogue with each other. The Linx senses when the wearer is coming to a standstill and automatically locks the joints in position. When the wearer is ready to start walking again, the sensors unlock the joints. The fine-tuning of the settings is facilitated by a Bluetooth connection between the limb and a mobile device such as a smartphone or tablet.

8. Bionic arm controlled by sensors implanted in the brain
After years of research, the DARPA-funded LUKE (Life Under Kinetic Evolution) prosthetic arm has finally hit the markets. The LUKE arm was named after Luke Skywalker’s robotic appendage in the Star Wars movies. The prosthetic limb is controlled by sensors implanted in the brain and it transmits electrical impulses back to the sensory cortex in order to restore the user’s sense of touch. When the user’s arm is flexed or tensed, the bionic arm changes its grip and position. This is in contrast with other prosthetic arms, which are either manually adjusted by the wearer or controlled by buttons or switches. The LUKE also allows a much greater degree of movement and flexibility. The four motors located in the hand and fingers enable the wearer to receive feedback on how hard they grip, enabling them to hold anything from an egg to a glass of water and perform tasks like opening locks, brushing hair and picking up various small items. The fact that the wrist, elbow and shoulder are individually powered even enables the user to reach behind their back or over their head.

9. New cochlear implants enable the deaf to surpass the hearing
Unlike ‘regular’ hearing aids, a cochlear implant bypasses the damaged parts of the inner ear to stimulate the hearing nerves with electrical signals instead of vibration or sound waves. The sophisticated Cochlear Nucleus 6 implant system consists of a surgically placed device under the skin and a second, streamlined external portion – the wireless sound processor – that is positioned behind the ear. The microphone on the sound processor converts sounds into digital information that is transferred to the implant. The implant then sends electrical signals to the cochlea, where the hearing nerve fibres send them to the brain where they are converted into perceived sound. With the Cochlear Nucleus, those with hearing impairments can now be one up on hearing people as the high tech system enables them to tune out or amplify certain sounds, something hearing people are unable to do. With various types of remote control devices, users can change programs, volume settings, sound filters and sensitivity levels and adjust the telecoil settings for phone use without having to touch their sound processor. Thanks to the Cochlear Nucleus 6, the quiet world of the hearing impaired can now be filled with a myriad of possibilities.

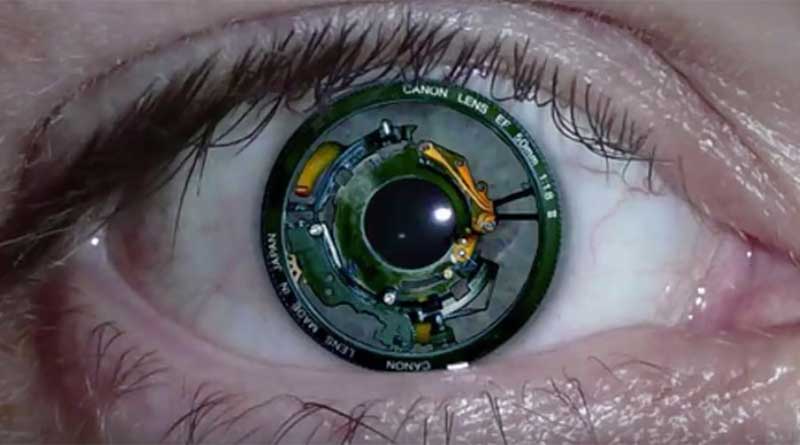
10. New bionic eye implant restores human sight
As part of the Orion 1 programme by Second Sight Medical, scientists made significant breakthroughs last year in restoring sight in a patient that had been blind for many years. Via a bionic implant – the Orion 1 visual cortical prosthesis device – which connects directly to the brain, the patient was able to see shapes and colours in the form of lines, spots and coloured flashes after signals were sent to the implant via a computer. This first human test of the implant was carried out by neurosurgeons of the University of California in Los Angeles (UCLA), lead by Dr. Nader Pouratian. According to Second Sight Medical chairman Robert Greenberg, the bionic eye system restores sight by stimulating the brain’s visual cortex, bypassing the optic nerve, and is designed for those who have gone completely blind as a result of glaucoma, diabetic retinopathy, cancer or injury. Stimulating the visual cortex in this way can greatly improve independence and quality of life for the visually impaired. Second Sight is looking forward to their first clinical trial of the complete Orion I system, which also includes a camera and glasses. The technology will provide a form of vision for the nearly six million blind people in the world who are not a candidate for the company’s Argus II retinal prosthesis, which only helps to restore visual perception in blind patients with retinitis pigmentosa.
Just the tip of the cyber
The breakthroughs discussed in this article are just a very small selection of the innumerable cyborg-esque technologies emerging every day. Some of them still require extensive testing, FDA approval and/or full integration into existing systems and procedures. But one thing is certain: technology will continue to provide us with new ways to save and improve lives and one day, whether in our own life or that of our children or grandchildren, we will all experience some level of cyborg-ness. Just wait and see.
Share via:


