- High-tech artificial limbs carry out the function of a lost limb
- Artificial eye mimics the structure of the human eye
- Inner and outer ear prosthetics
- Organoid skin from human stem cells and smart electronic sensory skin system
- Artificial thymus helps eliminate infections and cancerous cells
- Artificial wombs can give premature babies a better chance of survival
- Artificial ovaries restore cancer patients’ fertility
- Can an artificial heart make you feel ‘cold-hearted’?
- Bioartificial liver can significantly improve patient survival rates
- Artificial lungs will breathe for you when you can’t
- Artificial stomach and intestinal tract enable research into diseases
- Bionic pancreas takes over diabetes management
- Bioartificial kidney performs functions that dialysis can’t
- Neuralink to start human trials with brain implants
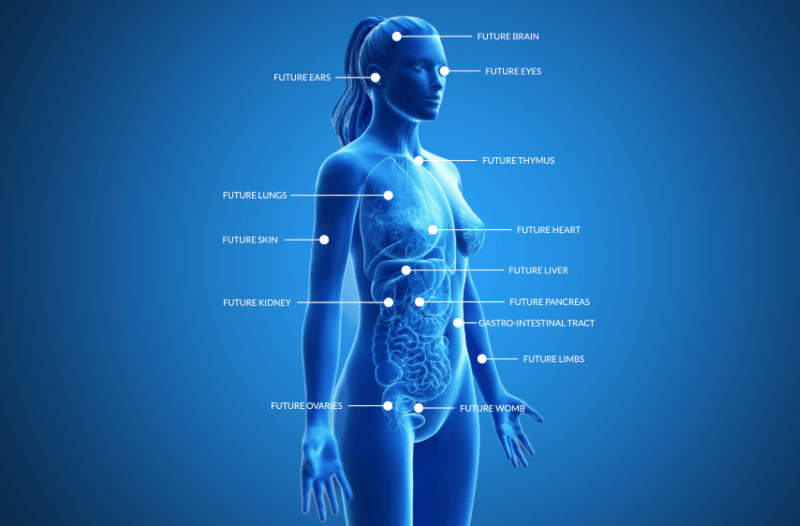
Body technology aims to repair, replace, or even outperform our natural body parts, ensuring ever increasing life expectancy. Artificial body parts that are created in high-tech labs and transplanted into the human body have been around for a number of years, but recent advances in medical technology have led to an explosion of innovation in this increasingly critical field, such as replacement organs and prosthetic limbs. According to trendwatcher and futurist Richard van Hooijdonk, “with our ability to enhance or repair the human body using advanced technology and (bio)artificial body parts, we have finally reached the point where we can save more and more lives, and potentially – in the future – even live on forever”.
LIMBS
High-tech artificial limbs carry out the function of a lost limb
Every year one million people worldwide lose (the function of) a limb. To make that more concrete – that’s equivalent to one amputation every thirty seconds. The value of the artificial limb market is expected to grow significantly, driven by accidents and worldwide increases of vascular disease, cancer, and diabetes. Losing control over a leg, foot, hand, or any other limb often means having to adjust to a completely new way of living. In America alone, approximately 2 million people live with amputations, with about 190,000 amputations performed every year. Using artificial limb prostheses, the performance of many regular activities – like eating, walking, and getting dressed – can be somewhat or even substantially restored.
According to György Lévay, research manager at Infinite Biomedical Technologies, the future of prosthesis will be increasingly scifi-like, and feature AI-powered prosthetics and even brain-controlled ones. “In one way or another, AI will be a part of advanced prostheses in the future. Processing the amount of data running between our brain and limbs will require smarter and smarter algorithms as the technology advances,” Lévay says. Bionic limbs – artificial limbs that use signals from the individual’s muscles or electrical signals from the brain and nerves to create movements – significantly improve mobility and are experienced more ‘as part of the person’s body’. They can, however, also lead to potential challenges, such as breakage of the implant, infection, implant instability, or bone fracture.

EYES
Artificial eye mimics the structure of the human eye
A new artificial eye prototype, developed by engineer Zhiyong Fan at Hong Kong University of Science and Technology, can be used for improved vision prostheses and humanoid robots, and almost brings cyborgs a step closer to reality. “Watching sci-fi series such as Star Trek and I, Robot, I thought about making a ‘super human eye’ to be used both in humanoid robots and for the visually challenged,” says Fan. The device mimics the structure of a real eye and, compared to the human eye, has an even faster reaction time, is nearly as light sensitive, and can see in dim light almost as well. The artificial eye registers changes in light within 40 milliseconds, as opposed to the human eye, which can take up to 150 milliseconds to do the same. The eye also produces images with clearer edges and greater contrast, compared to what a flat image sensor with a comparable amount of pixels can manage. The artificial eye even lacks a blind spot and is able to pick up a larger range of wavelengths. In the future, Fan hopes to be able to build prosthetic eyeballs in collaboration with medical researchers based on the design of his team. “The resulting biomimetic eye prototype has 30 times more sensors on the artificial retina than the real human eye. This super human eye technology, with high imaging resolution, will be ready for integration into medical robots to take care of patients. It will even cater to the visually impaired when we find suitable biocompatible materials,” says Fan.
And while the eye is already quite impressive, it does need quite a bit more work. Jessy Dorn, vice president of clinical and scientific affairs at biomedical company Second Sight, who works on retinal prostheses like the Argus II, points out that developing Fan’s electronic interface is only the first step. She says: “[The study authors] don’t talk about how it could possibly be connected to the human visual system. Such a device will need to interact with the human brain to produce images. That’s one of the bigger challenges, how to get any kind of high-resolution interface safely and reliably implanted and then to work with the human visual system.”
EARS
Inner and outer ear prosthetics
For many people suffering from severe or even full hearing loss, cochlear implants can significantly change lives. These implants bypass the damaged portions of the ear, directly stimulate the auditory nerve, and provide a sense of sound via a microphone and electronics behind the ear. Signals generated by the implant are sent via the auditory nerve to the brain, where these signals are recognised as sound. While hearing via a cochlear implant takes time to get used to, as it is not the same as normal hearing, it does enable many people to understand speech and various other sounds in their surroundings.
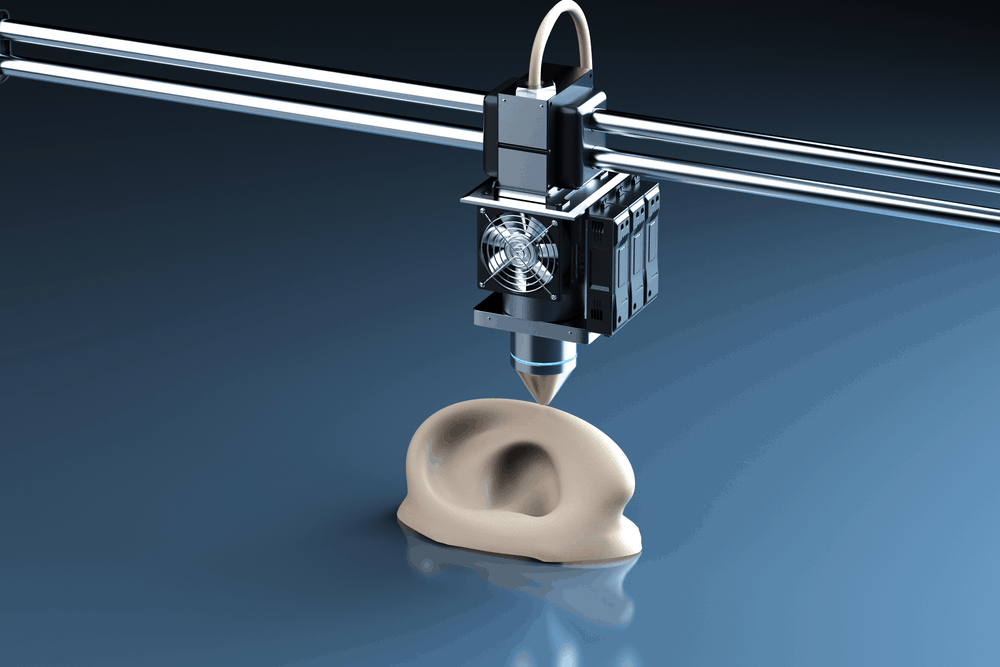
And in the case of outer ear trauma, for instance as a result of an accident or microtia (a congenital deformity where the external ear does not fully develop), a craniofacial prosthesis may be a solution. A team of scientists from Massachusetts General Hospital, lead by Thomas Cervantes and assisted by a plastic surgeon, created such an artificial ear, shaped like a human one, but made with a 3D printer using cartilage from sheep ears. According to the researchers, “the technology is now under development for clinical trials, and thus we have scaled up and redesigned the prominent features of the scaffold to match the size of an adult human ear and to preserve the aesthetic appearance after implantation.” The development of this outer ear prosthesis marks a significant step forward in the treatment of microtia.
SKIN
Organoid skin from human stem cells and smart electronic sensory skin system
The most success we’ve had so far creating artificial skin has been the production of epidermis, the outermost of the three layers that our skin is made up of, with the inner layers being the dermis and hypodermis. This technique is used in hospitals across the world and has saved the lives of tens of thousands of burn patients. For more extensive, deeper skin damage, no treatment was available until last year. In 2020, Karl Koehler, a neuroscientist, stem cell biologist, and organ regeneration ‘enthusiast’, as he calls himself, together with his team at the Boston Children’s Hospital, managed to lab-grow the full thickness of the skin instead of only the outermost layer. What the team created is best described as an organoid culture system that generates complex skin – akin to foetal facial skin and hair – from human stem cells. “This is the first study to show that human hair can be grown completely from stem cells in a dish, which has been a goal of the skin biology community for decades. We’ve developed a new cooking recipe for generating human skin that produces hair follicles after about 70 days in culture,” says Koehler. “This could be a huge innovation, providing a potentially unlimited source of soft tissue and hair follicles for reconstructive surgeries,” adds Dr Jiyoon Lee, also from Boston Children’s Hospital.
Researchers from Stanford University and Pohang University of Science and Technology (POSTECH) in South Korea have developed a fully artificial, electronic smart skin system that can detect movement as well as temperature simultaneously. The multimodal ion-electronic skin system could be used to restore some sense of touch in people who have lost that ability. Apart from temperature, the flexible, stretchy skin can detect sensations like pushing, twisting and pinching. “When an index finger touches an electronic skin, the electronic skin detects contact as a temperature change, and when a finger pushes the skin, the back part of the contact area stretches and recognises it as movement. I suspect that this mechanism is one of the ways that the actual human skin recognises different stimuli like temperature and movement,” says Insang You, a professor at POSTECH. To create an artificial smart skin system with the ability to detect movement and temperature simultaneously, the researchers created the sensor system in such a way that it can conduct ions – using electrolytes – similarly to how this happens in human skin. The ultimate objective is to develop artificial ion-electronic skin that simulates human tactile receptors and neurotransmitters. This could be used for medical applications and help restore the sense of touch in patients who have lost their tactile sensation as a result of an accident or illness. The researchers aim to apply this smart skin technology to humanoid skin and wearable devices.
THYMUS
Artificial thymus helps eliminate infections and cancerous cells
Researchers at the Francis Crick Institute and University College London (UCL) have used human stem cells and a bioengineered scaffold to construct an artificial thymus. This organ is critical in the immune system and develops T lymphocytes – cells that destroy or fight off infections or cancerous cells. Transplanted into patients born without this organ, which makes them critically susceptible to infections, the artificial thymus could help them lead a more normal life. The researchers are also considering the artificial thymus for the alleviation of transplant rejection. For instance, if a thymus is grown from the cells of an organ donor, the new thymus could also be transplanted into the patient receiving the donor organ to prevent organ rejection. This would eliminate the need for lifelong immune-suppression medication. According to Sara Campinoti, a researcher at the Crick Institute’s epithelial stem cell biology and regenerative medicine laboratory, “showing it is possible to build a working thymus from human cells is a crucial step towards being able to grow thymi which could one day be used as transplants.”
WOMB
Artificial wombs can give premature babies a better chance of survival
An artificial womb, named the biobag, was introduced in 2017 by a team at the Children’s Hospital of Philadelphia (CHOP). The team, consisting of a neonatologist, developmental physiologist, and surgeon created this prototype artificial womb to give extremely premature babies a greater chance of survival. Worldwide, extreme prematurity is the leading cause of infant morbidity and mortality. Babies born before 22 weeks often don’t survive, and even at 22 weeks their chances are still a very slim 10 per cent. A mere two weeks later, however, survival rates significantly increase – to up to 60 per cent. The team first managed to find a way to gestate sheep foetuses outside of the ewes’ womb. This has been a significant accomplishment, as sheep have a long gestation period, like humans, and the size of their foetuses are similar to ours. The biobag functions like an amniotic sac filled with warm, lab-created fluid. The lamb swallows and breathes this. The biobag contains an artificial placenta – an oxygenator that also provides nutrients and removes carbon dioxide – which is plugged into the umbilical cord of the lamb. And just like in a natural womb, the blood is pumped by the beating of the foetus’s heart. Over the weeks the lambs had been in the biobags, they continued to develop. After being removed from the biobag, they grew up normally.
In 2019, Dutch researchers at Eindhoven University of Technology received €2.9 million in funding from the Horizon 2020 EU Programme, to be invested in the development of a prototype artificial human womb for use in clinics. In the artificial wombs, premature human babies will be surrounded by fluids, and receive nutrients and oxygen through an artificial placenta connected to their umbilical cord. Guid Oei, a gynaecologist at the Maxima Medical Centre and professor at the Dutch university, says: “When we put the lungs back under water then they can develop, they can mature, but the baby will receive the oxygen by the umbilical cord, just like in the natural womb.” The prototype – of which a working version should be completed in 2024 – will be developed using 3D printed ‘human babies’ fitted with a myriad of sensors, enveloped by a complete recreation of the human womb. “When they are in this environment, they just feel, and see, and smell, and hear the same sounds as when they are in the womb of the mother, including her heartbeat,” says Oei.

OVARIES
Artificial ovaries restore cancer patients’ fertility
Up until recently, (young) women who are diagnosed with cancer and receive treatment only have a chance at pregnancy if their ovarian tissue is removed, frozen and – after having recovered – reimplanted. Certain types of cancer can, however, penetrate this tissue, which means the disease will find its way back into the body when reimplanted. Completely replacing the tissue with an artificial ovary would be the safest option, as it would restore the patient’s fertility and prevent potential re-introduction of the cancer. A team of engineers, materials scientists, gynaecologists, and natural scientists at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) have been researching groundbreaking techniques for developing artificial ovaries for these patients and helping them fall pregnant, despite the adverse effects chemotherapy has on their fertility.
The team used a method called electrospinning, which enables the use of a myriad of natural and synthetic polymers to create a scaffold of very thin fibres. This scaffold mimics the natural shape and structure of the ovarian cortex. The researchers tested the scaffold as a substrate for the adhesion of follicles from pigs’ ovaries. After ten days of culture, high numbers of viable follicles in the scaffold had retained their original shape. “This is an important step towards an ideal artificial ovary that imitates the natural organ in terms of environmental conditions for the growth and maturity of follicles. These results are very promising, but further research is required before any further development towards clinical applications can be made,” according to the research team.
HEART
Can an artificial heart make you feel ‘cold-hearted’?
The world’s biggest killer is heart disease and, in the very worst cases, the only thing that can save a life is a transplant. The problem is, however, that more hearts fail than donor hearts are available, and donor organ waiting lists are long. The French company Carmat has recently developed an artificial heart to help people during the time they are waiting for donor hearts. Weighing 4 kilograms, the surgically implanted ‘total artificial heart’ has a similar shape to a human heart. It is powered by batteries that provide approximately four hours of charge, contains sensors that detect blood pressure, and its blood flow is controlled by an algorithm in real-time. Carmat CEO Stéphane Piat says: “It works like a human heart so if the patient walks, the blood flow increases and if the patient is at rest, the blood flow is stable and low.” To minimise the risk of rejection and other adverse reactions, the parts of the heart that come into contact with the blood are created from material that is compatible with the patient’s body. The device has already been implanted in nineteen male patients – the current design is, unfortunately, too large for implantation in female patients. Other artificial hearts on the market, like the one made by SynCardia, have a fixed heart rate, instead of one that adjusts to the patient’s activity levels. Although Carmat wants to initially launch its devices for temporary use – in the case of patients waiting for a transplant – the company’s long-term objective is to create artificial hearts for permanent use.
While impressive and life-saving, could having an artificial heart also change how a patient perceives the world, relationships, and life in general? One person who lived with an experimental artificial heart for seven years, Jungian psychologist Peter Houghton, reported feeling less sympathetic and even somewhat ‘coldhearted’ towards other people. He mentions, for instance, wanting to connect with his grandchildren, while at the same time not “wanting to be bothered to have a reasonable relationship with them”, and not understanding the reason for this. Houghton says: “My emotions have changed. Somehow I can’t help that. I would describe myself as less intuitive. More of a thinking, more rational, less intuitive person.” Why Houghton experiences these emotions is unknown. It could be the lingering effects of the major surgery, the machinery itself, or the fact that the human brain is naturally optimised to get oxygen in pulse-driven spurts, instead of continuous pressure. All things considered, being saved from death, and “being transformed into a symbol for cyborg life while experiencing serious psychological transformations has been quite an experience,” says Houghton.
LIVER
Bioartificial liver can significantly improve patient survival rates
While our liver has the most extensive regenerative capacity of all our organs, when it is diseased or injured to such an extent that it’s unable to repair itself, patients quickly run out of options. Acute liver failure (ALF) is characterised by liver dysfunction, often followed by multiple organ system failure. Patients with ALF have a 80-90 per cent mortality rate. The most effective treatment is liver transplantation but, because of the long donor organ waiting lists, many patients don’t make it. A group of researchers, led by Dr Scott Nyberg, liver transplant surgeon and principal investigator in the Artificial Liver and Liver Transplantation Laboratory at the Mayo Clinic, are creating a Spheroid Reservoir Bioartificial Liver (SRBAL), a device that contains pig liver cell spheroids used to replace the liver function of the patient. The artificial liver has already been successful in supporting pigs with acute liver failure, and the objective of the device is to bridge the gap for patients suffering from liver failure who are waiting for a donor liver. The device is ultimately envisioned to support healing and regeneration of the diseased or injured liver, improving patient survival rates without the need for a transplant. Dr Nyberg’s team continues research into whether the artificial liver could be used to function similarly to a kidney dialysis device. “There’s a lot of work to be done, but this is a promising solution to the donor organ shortage in some cases,” says Dr Nyberg.
LUNGS
Artificial lungs will breathe for you when you can’t
Artificial lungs, or ‘microfluidic oxygenators’, can support patients with respiratory distress suffering from low blood oxygen levels. Acute respiratory distress can occur in anyone, from premature babies to adults with lung disease or severe COVID-19. Only in very severe cases can mechanical ventilation – during which oxygen gas is forced into the lungs – provide support, but this is not without complications. Technology that can introduce oxygen into the blood in alternative ways, albeit for short periods of time, is generally used as part of the heart-lung machine during cardiac surgeries. This ECMO (extra corporeal membrane oxygenation) technology has also been used to support SARS patients with acute respiratory distress.
Medtronic, a global medical technology leader that develops device-based medical therapies and services, is temporarily modifying its product indications so that health providers can use the company’s ECMO technology to treat people with severe cases of COVID-19. The company’s ‘artificial lung’ pumps blood from a patient’s body to an oxygenator, a device that facilitates long-term oxygen and carbon-dioxide transfer. The Medtronic devices can provide up to 6 hours of support and potentially reduce or eliminate the need for mechanical ventilation.
GASTRO-INTESTINAL TRACT
Artificial stomach and intestinal tract enable research into diseases
The Warsaw University of Life Sciences in Poland is home to a dynamic SHIME2 model of the artificial gastrointestinal tract – the first of its kind. The model enables the lifelike imitation and monitoring of the processes in the stomach, small intestine, and large intestine. The artificial digestive tract will be used for research into the microbiota of children, adults, and the elderly. The model will also be used to perform a wide range of experiments, such as the metabolism of dietary components and research into the impact of probiotic food.
Great strides have also been made in the development of mini stomachs from gastric organoids – minuscule clusters of human gastric tissue. This could enable new research into cancer, diabetes, and ulcers. According to Jim Wells, a researcher in developmental biology at the Cincinnati Children’s Hospital Medical Centre in the US, “there hasn’t really been a proper way to study diseases of the stomach. The human stomach is very different from animal stomachs. But with the pluripotent stem cells we can even grow transplant tissue. The challenge has been to get the cells to ‘differentiate’ – turn into cells for specific organs.” While still in their early stages of development and currently a good testbed for studying disease, these gastric organoids could one day be used as replacement tissue to repair the damage done by ulcers and even to create complete stomachs.
PANCREAS
Bionic pancreas takes over diabetes management
Diabetes patients typically manage their illness by continuously monitoring their blood glucose levels, and administering insulin when necessary. In terms of management, diabetes is one of the most challenging chronic diseases that requires continuous careful monitoring. The danger of administering too much insulin, for instance, is that it can lead to hypoglycaemia or low blood sugar. This can result in seizures, coma, and even death. The iLet – a name inspired by islet cells in the pancreas – is a pocket-sized, wearable medical device that helps patients with type 1 diabetes autonomously control blood glucose levels, similar to an insulin pump. But unlike insulin pump therapy, patients using the iLet don’t need to count carbohydrates, enter insulin delivery rates, or administer extra insulin for corrections. All they have to do is enter their body weight and the bionic pancreas will initialise therapy.
According to president and CEO of iLet manufacturer Beta Bionics, Edward R Damiano, “the iLet Bionic Pancreas System represents a true breakthrough therapy for the management of glycemia, particularly in type 1 diabetes. We are particularly excited by the possibility that the iLet may be able to provide safer and more effective therapy in far more people than current therapies due to its simplicity of use.” The iLet can function as three devices: a glucagon-only bionic pancreas, an insulin-only bionic pancreas, or a bihormonal bionic pancreas using glucagon and insulin. Using a wireless glucose sensor worn by the patient that monitors blood sugar levels at 5-minute intervals, the device determines which hormone is needed and administers it to the patient via catheters. According to data from in-home studies, presented at the American Diabetes Association’s Scientific Sessions, the use of the bionic pancreas showed significantly improved reductions in mean glucose and hypoglycaemia compared to the use of conventional insulin pump therapy.
KIDNEY
Bioartificial kidney performs functions that dialysis can’t
Nearly 2 million people worldwide suffer from end-stage renal disease, which is the most severe form of kidney disease. As the characteristics and the function of kidneys could easily be compared to a complex biology and chemistry lab, it’s no surprise that there hasn’t been much progress in the treatment of patients with kidney failure. However, the San Francisco-based John & Marcia Goldman Foundation recently awarded The Kidney Project, headquartered at the UCSF (University of California San Francisco), a $1 million grant for the continued development of its bioartificial kidney. This revolutionary artificial kidney will be implanted in the abdomen, perform essential functions that dialysis treatments are unable to, and eliminate the need for immunosuppressant medication. The bioartificial kidney’s bioreactor contains kidney cells that will help filter a patient’s blood. It will do this by reabsorbing nutrients and making sure that toxins and excess water (urine) are routed to the bladder. The device will also assist with hormone production and the regulation of blood pressure, which is something that regular dialysis treatments don’t do. The use of the artificial kidney will put an end to the cumbersome and costly chronic dialysis process that has been the standard treatment since the 1950s. According to John and Marcia Goldman, “people struggling with dialysis need and deserve better choices. The Implantable Artificial Kidney will allow those with end stage renal disease to lead more normal lives, freed from grueling dialysis sessions that take a toll physiologically, psychologically, and financially. Dialysis is a short-term treatment; The Kidney Project is offering a life-long option.”
BRAIN
Neuralink to start human trials with brain implants
Neuralink – Elon Musk’s neurotechnology company – has recently advanced its microchip technology in such a way that a monkey with a chip implant can now play video games with its mind. Mind you, this is not the first time an animal was given a Neuralink trial implant. In 2020, a pig named Gertrude received a brain-monitoring chip that enabled scientists to wirelessly monitor the animal’s brain activity. During a presentation showing Gertrude snuffling around her pen, the audience could hear the beeping sounds from the pig’s brain-computer interface. When asked whether the technology could eventually enable users to save and replay memories, Musk replied: “Yes, I think in the future you’ll be able to save and replay memories. I mean, this is obviously sounding increasingly like a Black Mirror episode. But… well, I guess they’re pretty good at predicting. Essentially, if you have a whole brain interface, everything that’s encoded in memory you could upload. You could basically store your memories as a backup and restore the memories. Then ultimately you could potentially download them into a new body or into a robot body.”
Musk has claimed that the potential of the microchip is virtually limitless, and that it could even enable humans to compete with artificial intelligence. Matthew MacDougall, Neuralink’s head neurosurgeon, mentioned that they had so far only managed to implant the chip into the cortical surface of the brain. In the future, however, they hope to be able to go into deeper areas, such as the hypothalamus. This area is believed to play an important part in mental illnesses. Neuralink has been making incredible strides lately. The company is even planning human trials by the end of this year. During these trials, artificial intelligence (AI) will be implanted into human brains to study the technology’s ability to read and write brain activity. While Musk’s long-term goal seems to be to achieve some degree of symbiosis with AI, Neuralink’s short-term goals are quite a bit more grounded. According to Musk, the device could be used to retrain the areas of the brain that are responsible for causing anxiety, depression, and addiction. Brain-machine interfaces could also be used to assist people with neurological conditions to control devices like smartphones or computers with their brainwaves. He also hopes it could help cure paralysis and assist in the fight against Parkinson’s and Alzheimer’s. Musk said on Twitter: “Neuralink is working super hard to ensure implant safety & is in close communication with the FDA. If things go well, we might be able to do initial human trials later this year.”

In closing
While prosthetics and artificial organs have been around for a long time, over the years the vision of using technology to ‘build improved humans’ has resulted in continuous advances to develop better‐controlled, more lifelike, and more efficient bodies. What’s different about the new generation of body technology, according to futurist Richard van Hooijdonk, is its union with bionic technology, and how it combines fields as diverse as hydraulics, electronics, computing, biotechnology, nanotechnology, and medicine. Some of the breakthroughs discussed in this article are still in their developmental phase and either require extensive testing, regulatory approval, integration into existing procedures and systems, or any combination of the above. One thing is certain, however: technology will continue to provide us with new ways to save lives. In the future, we will be able to improve or even replace more and more body parts with their artificial or bionic counterparts. And with the incredible advances in the field of neurotechnology, our minds might even be able to live on long after our physical bodies have disappeared.
Share via:


