- Chinese surgeons are using brain implants to treat addiction
- Addicaid is an app that uses AI to help methamphetamine addicts stay sober
- Sober Grid uses AI to predict a relapse
- hc1 uses machine learning to spot patterns of abuse among people who use opioids
- inRecovery is a blockchain-powered addiction recovery platform
- Can technology help us fight drug abuse?
Drug abuse is a serious issue that affects millions of people around the world. It can have devastating consequences on a person’s life, leading to various infectious diseases and other health issues, crime, unemployment, homelessness, social exclusion, and even death. But drug abuse doesn’t just affect individuals, it affects society at large through reduced workforce productivity and costs associated with addiction treatment.
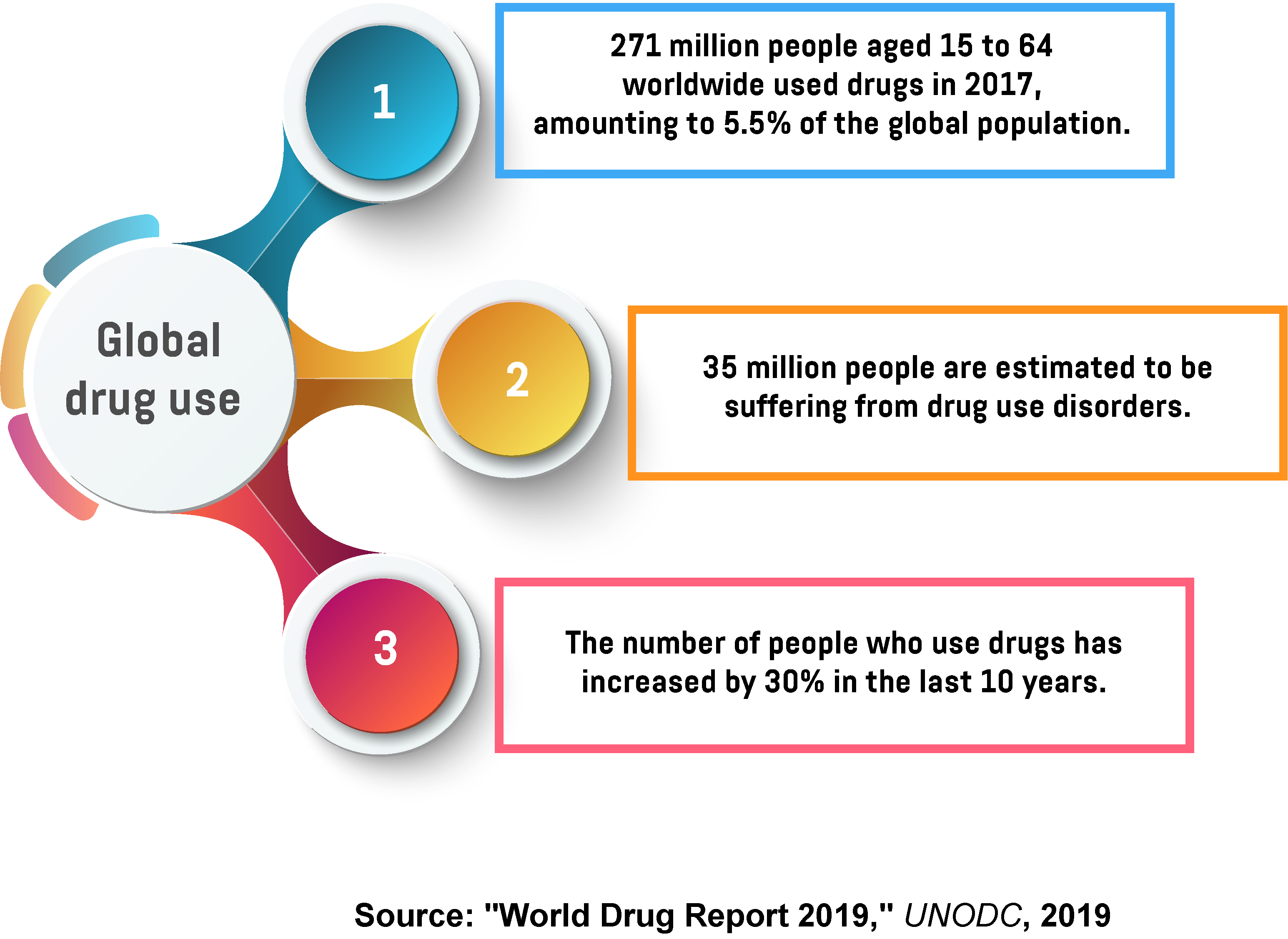
According to the UN’s World Drug Report 2019, around 271 million people worldwide used drugs in 2017, while 35 million suffer from drug use disorders. The report shows that the number of people who use drugs has increased by 30 per cent compared to a decade ago, but this increase can be partly attributed to improved research and more precise data, as well as the increase in the global population.
The UN report also reveals that the use of drugs was responsible for 585,000 deaths and 42 million years of ‘healthy’ life lost in 2017, with approximately two-thirds of those deaths attributed to opioids. Unfortunately, the majority of people with drug use disorders still lack access to adequate treatment, with just one in seven of them receiving the help they need. To address this growing problem and ensure that everyone gets access to proper care, medical professionals around the world are increasingly turning to technology.
Chinese surgeons are using brain implants to treat addiction
Researchers at the Ruijin Hospital in Shanghai recently announced the start of a new clinical trial that will attempt to treat methamphetamine addiction with deep brain stimulation (DBS). It’s a highly experimental procedure that involves drilling two small holes in a patient’s skull and implanting a device into their brain. The device is attached to the patient’s nucleus accumbens, a small structure near the base of the forebrain that’s been associated with addiction, where it works by stimulating targeted areas with electrical impulses, basically acting as a pacemaker for the brain.
Deep brain stimulation has been used to treat movement disorders like Parkinson’s in the past, but it remains a highly controversial subject. Its detractors believe it should be banned altogether, as the risks far outweigh any potential benefits. The problem is that we still don’t fully understand how DBS works or whether it has any positive effects. At this point, scientists aren’t even sure where exactly the electrodes should be placed to treat addiction. On the other hand, the risks are very real and include brain hemorrhage, seizures, infection, and personality changes.
Previously, two laboratories in the US tried to treat alcoholism with DBS. However, as the preliminary results failed to justify the risks, both clinical trials were eventually abandoned. “It would be fantastic if there were something where we could flip a switch, but it’s probably fanciful at this stage,” says Adrian Carter, who heads the neuroscience and society group at Monash University in Melbourne. “There’s a lot of risks that go with promoting that idea.”
Addicaid is an app that uses AI to help methamphetamine addicts stay sober
Overcoming any kind of addiction can be a grueling process, but that’s especially true for methamphetamine addiction. Years of meth abuse can cause serious damage to dopamine receptors in the brain, leading to a condition called anhedonia, which makes addicts unable to feel pleasure. Methamphetamine addicts often feel terribly ill during withdrawal, experiencing nausea, fever, sweat, and vomiting. Coupled with anhedonia symptoms, this can easily lead to depression and eventually relapse. Unfortunately, traditional methods haven’t proven particularly effective in treating meth addiction, with a dismal success rate of just 12 per cent. As a result, meth addicts are increasingly looking for innovative approaches, with artificial intelligence emerging as a promising solution.
Developed by Sam Frons, a recovering meth addict, Addicaid is an app that uses artificial intelligence in combination with clinical research to predict when a person may be about to relapse. In addition to this, the app also offers additional treatment suggestions, including cognitive behavioural therapy and phone numbers for various treatment lines and centres. For example, when the app detects a recovering alcoholic walking into a bar, it will immediately try to prevent a relapse by sharing phone numbers for them to call or suggesting strategies to help them stay sober.
These suggestions are personalised to meet each individual’s needs based on the information they shared with the app. This is especially important because recovery is different for each person and what works for one addict doesn’t necessarily have to work for others. In theory, this should make this approach more effective than traditional methods in helping meth addicts avoid a relapse.
Sober Grid uses AI to predict a relapse
Described as the world’s largest mobile sober community, Sober Grid is a free app that helps addicts find support by connecting them with resources and other people who are going through the same thing. The app has more than 120,000 users in various stages of the recovery process, ranging from those who are just looking to start recovery to long-term members who use the app to offer support to others. Such a large user base has allowed Sober Grid to collect a great deal of data about the recovery process over the years, including when exactly relapses happen and the type of communication that precedes them. This inspired the following idea: what if there was a way to create an algorithm that would be able to use this data to predict the next relapse?
Sober Grid recently joined forces with researchers from the University of Pennsylvania to create an algorithm that uses AI to analyse the language used by the app’s users to predict future relapses and intervene before it’s too late. “The words people use reflect who they are (e.g. their personality) and how they feel (e.g. happy, depressed, stressed, relaxed). People using Sober Grid post messages and indicate the number of days they have been sober. We then build statistical models to predict sobriety or relapse from the frequencies with which words are used,” says Lyle Ungar, a professor of computer and information science at the University of Pennsylvania and a co-investigator on the project.
Of course, all of the information used in the project is de-identified so that it can’t be traced back to any individual. Once the algorithm detects that a person is likely to relapse, it will immediately offer support in the form of short mindfulness modules or cognitive behavioural therapy, or put them in touch with one of the available trained coaches. The service is entirely opt-in, presenting users only with those options they’ve explicitly signed up for.
hc1 uses machine learning to spot patterns of abuse among people who use opioids
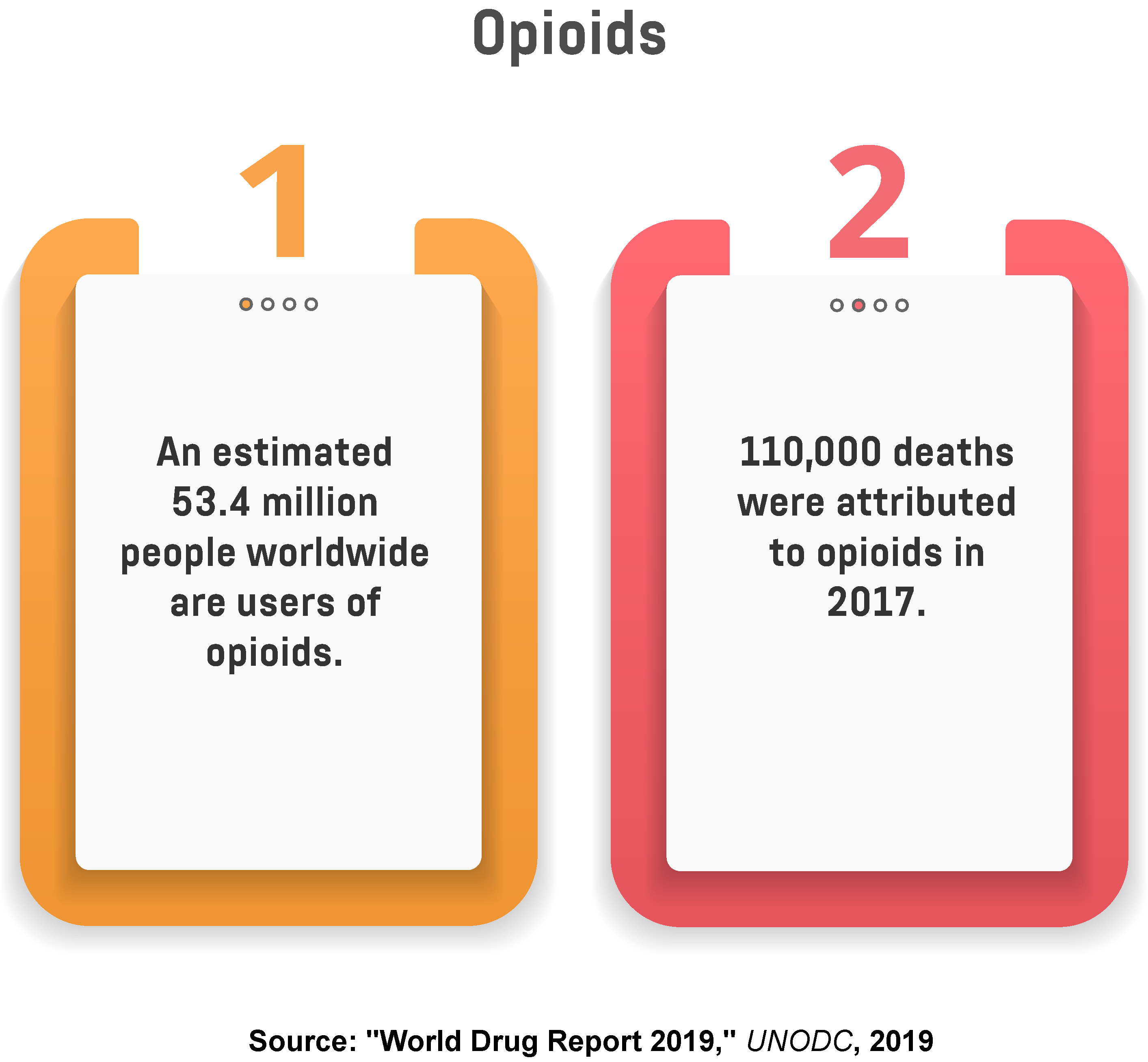
According to UN’s World Drug Report 2019, there are approximately 53.4 million people worldwide who use opioids, with 110,000 deaths attributed to this class of drugs in 2017.
With an estimated 53.4 million users and 110,000 deaths attributed to opioids in 2017, this class of drugs continues to pose the biggest health risk for its users. Usually prescribed to people who are dealing with chronic headaches and backaches, recovering from surgery, or going through cancer treatment, opioids are highly addictive substances with great potential for misuse. To address this growing problem and prevent substance abuse, the Indiana-based software company hc1 developed a platform called Opioid Dashboard, which uses machine learning technology to spot patterns of misuse and abuse among people who use opioids.
To create the platform, hc1 partnered with drug-testing labs from all over the United States and used their de-identified data to train its machine learning algorithms to identify potential patterns. This allowed the company to create a massive database that includes more than 90 million user profiles, which could be used to help healthcare organisations deliver a better, more personalised service. For example, the platform can now analyse the number of prescriptions written in a state to determine whether there’s any correlation between prescription volume and misuse, but the company hopes it will one day be able to not just detect existing patterns, but also predict future behaviour.
“We use machine learning to generate a view into what’s happening across America,” says Brad Bostic, the CEO of hc1. “It’s an early warning system. We can see leading indicators that allow us to predict where to put resources to lower the misuse of opioids. Federal and state governments are deploying funds to reduce opioid use, but it’s very hard to measure impact. If we can look by county or ZIP code, it really helps to say whether an investment in a population is lowering misuse and abuse.”
inRecovery is a blockchain-powered addiction recovery platform
Recovery is an incredibly complex process that consists of numerous steps, such as drug screenings, therapy sessions, medical prescriptions, monitoring of vitals, and various group activities. With so many different activities and participants involved, maintaining a stable one-on-one connection with each individual patient can become challenging, reducing patient engagement and making the treatment less effective. inRecovery was created to address some of these issues and help addicts both with their sobriety and social reintegration.
It’s the world’s first addiction recovery platform powered by blockchain that was designed to increase patient engagement and improve treatment outcomes. The platform consists of several separate components. The inRecovery+ app employs a gamification model to encourage higher levels of engagement in patients by rewarding them with points for check-ins to therapy sessions, group activities, meetings, and drug screenings. Patients can also earn badges for outstanding behaviour, including perfect attendance, volunteering, career planning, and extracurricular activities.
Patients are guided through recovery by personalised Therapy Paths, which are created based on their addiction type and required level of care. Therapy Paths are powered by EMMA (Enhanced Machine Medicine for Addiction), an intelligence engine that uses machine learning and AI to create personalised therapy for each patient in real time. EMMA constantly monitors patients, suggest activities, and alerts therapists and rehab managers if it detects an elevated risk of relapse. All incidents are recorded on the inRecovery blockchain, which serves as the backbone of the entire platform. In addition to protecting patient privacy, blockchain also helps them reintegrate into society by providing them with a reliable report of their sobriety, which they can show to potential employers and landlords.
Can technology help us fight drug abuse?
As drug abuse continues to increase around the world, often with deadly consequences, healthcare professionals are increasingly looking for alternatives to traditional addiction treatment methods. While therapy and rehab can be an effective way to fight drug abuse, they’re not available to everyone, and only a small proportion of addicts actually get the help they so desperately need. In recent years, technology has emerged as a potential solution to this problem.
Technology has already transformed many different aspects of our lives and the same may soon be true for addiction treatment. Whether it’s implanting a device into a patient’s brain to help them control their urges, or using artificial intelligence and machine learning to monitor patients and predict when they may be about to relapse, technology is playing an increasingly important role in fighting drug abuse. While it remains to be seen whether it truly is the future of addiction treatment, anything that can help us deal with this deadly epidemic is welcome at this point.
Share via:


